Network Discrepancy Report
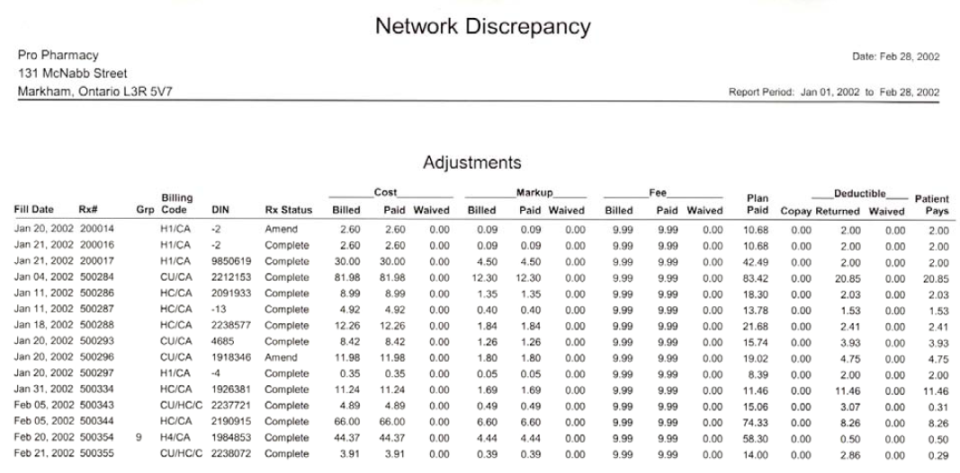
The Network Discrepancy Report provides the ability to review prescriptions that had adjustments in the price after being submitted for payment. It will include any prescriptions with differences in the cost, markup and/or fee, as well as prescriptions with deductibles. Claims paid in full, where no values were waived and the Patient Pays is $0.00, are not included on the report. Additionally, Cash prescriptions (i.e. where the billing code is CA) are not included in the report.
The Adjustment values are taken directly from the Claim Summary window in Rx Detail, therefore the values in the report can be compared against each prescription’s Claim Summary.
To view adjustments for a specific third party, a Third Party can be specified before generating the report. Once the report is generated, the name of the third party will be indicated near the top of the report.
The report can be sorted by prescription number or third party.
The report is broken into two sections: Adjustments and Rejections/Failures.
Adjustments Sample Report
Click on an area in the sample report to see a description of the field.
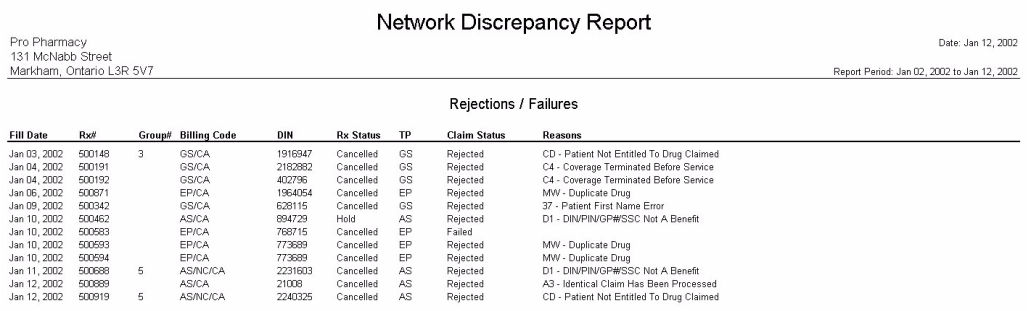
Rejections/Failures Sample Report
When the Rejected checkbox is selected in the Extended report criteria, the report will list all rejections and failures that occurred during the report period.
Click on an area in the sample report to see a description of the field.